Parkinson’s disease is a genetic disease that affects 1 in 100 people over the age of 60. This diagnosis is a life-changing event, that causes nerve cells, called neurons, in the brain to slowly die. Learn about gene therapy clinical trials and how they might offer hope for managing symptoms, improving the effects of existing medications, or potentially slowing or stopping disease progression.
About Parkinson's Disease
Symptoms - Parkinson’s disease causes nerve cells, called neurons, in the brain to slowly die. Neurons create a neurotransmitter called dopamine, which is a chemical messenger that sends messages from one nerve cell in the brain to another. Critically low levels of dopamine in the brain can negatively affect movement. This results in symptoms, such as tremors, trouble starting movements, slow movement, and impaired balance and coordination. People with Parkinson’s disease also face emotional and behavioral changes, including sleeping problems and depression. This makes life with the disease hard on both the people affected and their caregivers.
 Cause - The exact cause(s) are still unknown. However, recent studies have identified several genes that could put someone at risk for Parkinson’s disease. Many of these genes are important for proper lysosome function. Often referred to as the “recycling center” of cells, lysosomes break down and remove waste within cells. Without proper breakdown of these waste products, it is believed they build up and cause inflammation (swelling) and neurodegeneration (brain cell death). Mutations (changes or variants) in the GBA1 gene are now known to be the single largest genetic risk factor for developing Parkinson’s disease. Overall, the environmental and genetic factors that cause the disease—and their relationship between each other—are a major focus of research.
Cause - The exact cause(s) are still unknown. However, recent studies have identified several genes that could put someone at risk for Parkinson’s disease. Many of these genes are important for proper lysosome function. Often referred to as the “recycling center” of cells, lysosomes break down and remove waste within cells. Without proper breakdown of these waste products, it is believed they build up and cause inflammation (swelling) and neurodegeneration (brain cell death). Mutations (changes or variants) in the GBA1 gene are now known to be the single largest genetic risk factor for developing Parkinson’s disease. Overall, the environmental and genetic factors that cause the disease—and their relationship between each other—are a major focus of research.
Gene Therapy Approaches
Gene therapy aims to be given one-time and uses a viral vector to deliver a working gene into cells. Scientists know that viruses are good at getting into cells, so they have learned how to safely use this ability as a carrier to deliver working genes. But don’t worry, the viral genes are removed, so only therapeutic (intended) genes are delivered.
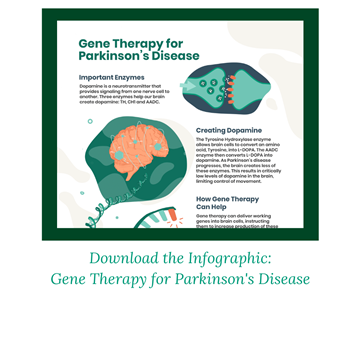
One approach being researched delivers a working DDC gene into cells to instruct them to make more AADC enzyme. As the disease progresses, not only does the brain create less dopamine, it also creates less of the AADC enzyme. The AADC enzyme helps brain cells convert an amino acid called L-DOPA into dopamine. Amino acids are molecules that combine to create proteins. L-DOPA is naturally occurring, or can be provided via an existing Parkinson’s medication. Without the AADC enzyme to help convert it into dopamine, L-DOPA has no effect. Gene therapy may be used together with existing medications for a stronger result by allowing the L-DOPA medication to then better regulate levels of dopamine in the brain.
Another gene therapy approach being studied has the potential to treat people with genetic forms of Parkinson’s disease. For example, some people with Parkinson’s disease have mutations in the GBA1 gene. This gene contains the instructions to produce an enzyme called beta-glucocerebrosidase (GCase) that is needed for cells to function properly. Gene therapy can be used to deliver a working copy of the GBA1 gene to help restore the GCase enzymes.
Current Treatments
There is no standard treatment, as every person has their own unique factors relating to their condition (age, mobility level, severity of symptoms, etc.). There are many medications available to manage symptoms that need to be taken regularly and adjusted as the disease progresses. However, none yet exist that can reverse the effects of the disease. It is very common for people with Parkinson’s disease to take a variety of these medications at once, in different combinations of doses and times of the day.
-
Levodopa, an oral medication that helps treat patients in the earlier stages of the disease, but has been shown to have weak results over time. As discussed earlier, the medication could potentially be more effective when paired with a gene therapy approach.
-
Some patients with advanced Parkinson’s disease may undergo a procedure called Deep Brain Stimulation, also known as DBS. In the case of DBS, a device implanted in the brain provides electrical impulses, helping the brain control some motor systems. Initial research has shown that patients with a DBS implant would still be eligible for gene therapy.
Treatment Pipeline
There are active gene therapy clinical trials for Parkinson’s. Clinical trials are part of a required research process to understand the way a drug or treatment will interact with the human body and whether it is safe and effective. This research and development is being done by companies including Axovant, Prevail Therapeutics, and Voyager Therapeutics. To stay up to date on open clinical trials in the U.S. or globally, visit the ASGCT Clinical Trials Finder and search using the "diagnosis" filter.
Participating in a Clinical Trial
 There is currently no cure for the disease, only medications to help manage symptoms, but those do not alter disease progression. Therefore, some people with poorly managed or unmanaged symptoms may consider an investigational gene therapy as an option. It is important to be informed when entering a clinical trial, so we introduce some key points below. Go to the considering a clinical trial page for more information and resources to help guide you.
There is currently no cure for the disease, only medications to help manage symptoms, but those do not alter disease progression. Therefore, some people with poorly managed or unmanaged symptoms may consider an investigational gene therapy as an option. It is important to be informed when entering a clinical trial, so we introduce some key points below. Go to the considering a clinical trial page for more information and resources to help guide you.
-
Eligibility - Eligibility for a trial is based on strict inclusion and exclusion criteria. These are specific factors that determine whether a person can or cannot join a clinical trial. This is an important way for researchers to understand if the gene therapy is working properly and to ensure participant safety. These criteria may be different for different trials but can include factors such as age, how advanced the disease is, medical history, genetic status, travel abilities and more. Speak with a movement disorder specialist or a member of the clinical trial research team to help determine if you or your loved one may be eligible for a clinical trial. Visit the International Parkinson and Movement Disorder Society’s movement disorders specialist directory to find one in your area.
-
Risks – As with any medical intervention, there are risks that need to be carefully considered. Before participating in a clinical trial, a member of the research team should review any potential risks and benefits with the patient or caregiver. Therapies being studied in clinical trials are not a guaranteed cure and cannot guarantee beneficial results. There is always a chance that the investigational treatment may not work. In the event a person is not satisfied with the outcome, the person cannot be given another dose of the same gene therapy. In addition, participating in a clinical trial may prevent future participation in other trials or from receiving other types of treatments. Gene therapy can be an alteration for the lifetime, so people should be aware that there could be long term effects (both good or bad) that are unknown at this time.
-
Benefits – Participating in a trial may offer many potential benefits compared to not receiving any form of intervention for a fatal disease. Gene therapy aims to be a one-time treatment with lasting positive effects to slow or stop disease progression for a lifetime, or better manage symptoms, but again there is no guarantee. This is possible because it targets the cause of disease, which is a faulty gene. If gene therapy is received earlier in the course of disease, it has the potential to stop any damage before it occurs.
-
Long-term follow up – It is the patient’s responsibility to comply with the long-term follow-up of a trial. FDA guidelines require the clinical trial research team to monitor safety and potential long-term effects of a gene therapy. Follow-up may require in-person appointments that vary in frequency and location, or completion of mailed packets with response forms. The need for long-term data collection for a gene therapy trial can last up to 15 years—another reason to consider all outcomes and responsibilities that come with committing to a clinical trial. There are a limited number of participants in trials so a lack of attendance at follow-up appointments leads to not enough study data. This could negatively affect FDA approval of a new drug and thereby limit access to the therapy by patients who did not participate in the clinical trial.
Access
At this time, we do not know if or when gene therapies will be approved by the FDA and commercially available for people living with Parkinson’s disease. The overall process may take several more years, until it is deemed safe and effective by the FDA.
Stay Informed
 There are many patient advocacy organizations to follow or get involved with. They work hard to fund research and advocate for patient and family needs. They are also a great way to connect with others affected by the disease if you are looking for support and advice.
There are many patient advocacy organizations to follow or get involved with. They work hard to fund research and advocate for patient and family needs. They are also a great way to connect with others affected by the disease if you are looking for support and advice.
Was this information helpful? If so, please share! All ASGCT Patient Education resources are free to use by sharing on social media, embedding the video, or simply linking to this page! Please credit the American Society of Gene and Cell Therapy or Tag @ASGCTherapy.